PHILIPSBURG, Mont. — On a recent day in this 19th-century mining town turned tourist hot spot, students made their way into the Granite High School lobby and past a new filtered water bottle fill station.
Water samples taken from the drinking fountain the station replaced had a lead concentration of 10 parts per billion — twice Montana’s legal limit for schools of 5 parts per billion for the toxic metal.
Thomas Gates, the principal and superintendent of the small Philipsburg School District, worries the new faucets, sinks, and filters the district installed for roughly 30 water sources are temporary fixes. The high school, built in 1912, is likely laced with aged pipes and other infrastructure, like so much of this historic town.
“If we change faucets or whatever, lead is still getting pushed in,” Gates said.
The school in Philipsburg is one of hundreds in Montana grappling with how to remove lead from their water after state officials mandated schools test for it. So far, 74% of schools that submitted samples found at least one faucet or drinking fountain with high lead levels. Many of those schools are still trying to trace the source of the problem and find the money for long-term fixes.
In his Feb. 7 State of the Union address, President Joe Biden said the infrastructure bill he championed in 2021 will help fund the replacement of lead pipes that serve “400,000 schools and child care centers, so every child in America can drink clean water.”
However, as of mid-February, states were still waiting to hear how much infrastructure money they’ll receive, and when. And schools are trying to figure out how to respond to toxic levels of lead now. The federal government hasn’t required schools and child care centers to test for lead, though it has awarded grants to states for voluntary testing.
During the past decade, nationwide unease has been stirred by news of unsafe drinking water in places like Flint, Michigan. Politicians have promised to increase checks in schools where kids — who are especially vulnerable to lead poisoning — drink water daily. Lead poisoning slows children’s development, causing learning, speech, and behavioral challenges. The metal can cause organ and nervous system damage.
A new report by advocacy group Environment America Research & Policy Center showed that most states fall short in providing oversight for lead in schools. And the testing that has happened to this point shows widespread contamination from rural towns to major cities.
At least 19 states require schools to test for lead in drinking water. A 2022 law in Colorado requires child care providers and schools that serve any kids from preschool through fifth grade to test their drinking water by May 31 and, if needed, make repairs. Meanwhile, California leaders, who mandated lead testing in schools in 2017, are considering requiring districts to install filters on water sources with high levels of lead.
As states boost scrutiny, schools are left with complicated and expensive fixes.
As it passed the infrastructure bill, Congress set aside $15 billion to replace lead pipes, and $200 million for lead testing and remediation in schools.

White House spokesperson Abdullah Hasan didn’t provide the source of the 400,000 figure Biden cited as the number of schools and child care centers slated for pipe replacement. Several clean-water advocacy organizations didn’t know where the number came from, either.
Part of the issue is that no one knows how many lead pipes are funneling drinking water into schools.
The Environmental Protection Agency estimates between 6 million and 10 million lead service lines are in use nationwide. Those are the small pipes that connect water mains to plumbing systems in buildings. Other organizations say there could be as many as 13 million.
But the problem goes beyond those pipes, said John Rumpler, senior director for the Clean Water for America Campaign at Environment America.
Typically lead pipes connected to public water systems are too small to serve larger schools. Water contamination in those buildings is more likely to come from old faucets, fountains, and internal plumbing.
“Lead is contaminating schools’ drinking water” when there aren’t lead pipes connecting to a municipal water source, Rumpler said. Because of their complex plumbing systems, schools have “more places along the way where lead can be in contact with water.”
Montana has collected more data on lead-contaminated school water than most other states. But gaps remain. Of the state’s 591 schools, 149 haven’t submitted samples to the state, despite an initial 2021 deadline.
Jon Ebelt, spokesperson with the Montana Department of Public Health and Human Services, said the state made its deadline flexible due to the COVID-19 pandemic and is working with schools that need to finish testing.
Greg Montgomery, who runs Montana’s lead monitoring program, said sometimes testing stalled when school districts ran into staff turnover. Some smaller districts have one custodian to make sure testing happens. Larger districts may have maintenance teams for the work, but also have a lot more ground to cover.
Outside Burley McWilliams’ Missoula County Public Schools office, about 75 miles northwest of Philipsburg, sit dozens of water samples in small plastic bottles for a second round of lead testing. Director of operations and maintenance for the district of roughly 10,000 students, McWilliams said lead has become a weekly topic of discussion with his schools’ principals, who have heard concerns from parents and employees.
Several of the district’s schools had drinking fountains and classroom sinks blocked off with bags taped over faucets, signs of the work left to do.
The district spent an estimated $30,000 on initial fixes for key water sources by replacing parts like faucets and sinks. The school received federal COVID money to buy water bottle stations to replace some old infrastructure. But if the new parts don’t fix the problem, the district will likely need to replace pipes — which isn’t in the budget.
The state initially set aside $40,000 for schools’ lead mitigation, which McWilliams said translated to about $1,000 for his district.
“That’s the one frustration that I had with this process: There’s no additional funding for it,” McWilliams said. He hopes state or federal dollars come through soon. He expects the latest round of testing to be done in March.
Montgomery said Feb. 14 that he expects to hear “any day now” what federal funding the state will receive to help reimburse schools for lead mitigation.
Back in Philipsburg, Chris Cornelius, the schools’ head custodian, has a handwritten list on his desk of all the water sources with high lead levels. The sink in the corner of his office has a new sign saying in bold letters that “the water is not safe to drink.”
According to state data, half the 55 faucets in the high school building had lead concentrations high enough to need to be fixed, replaced, or shut off.
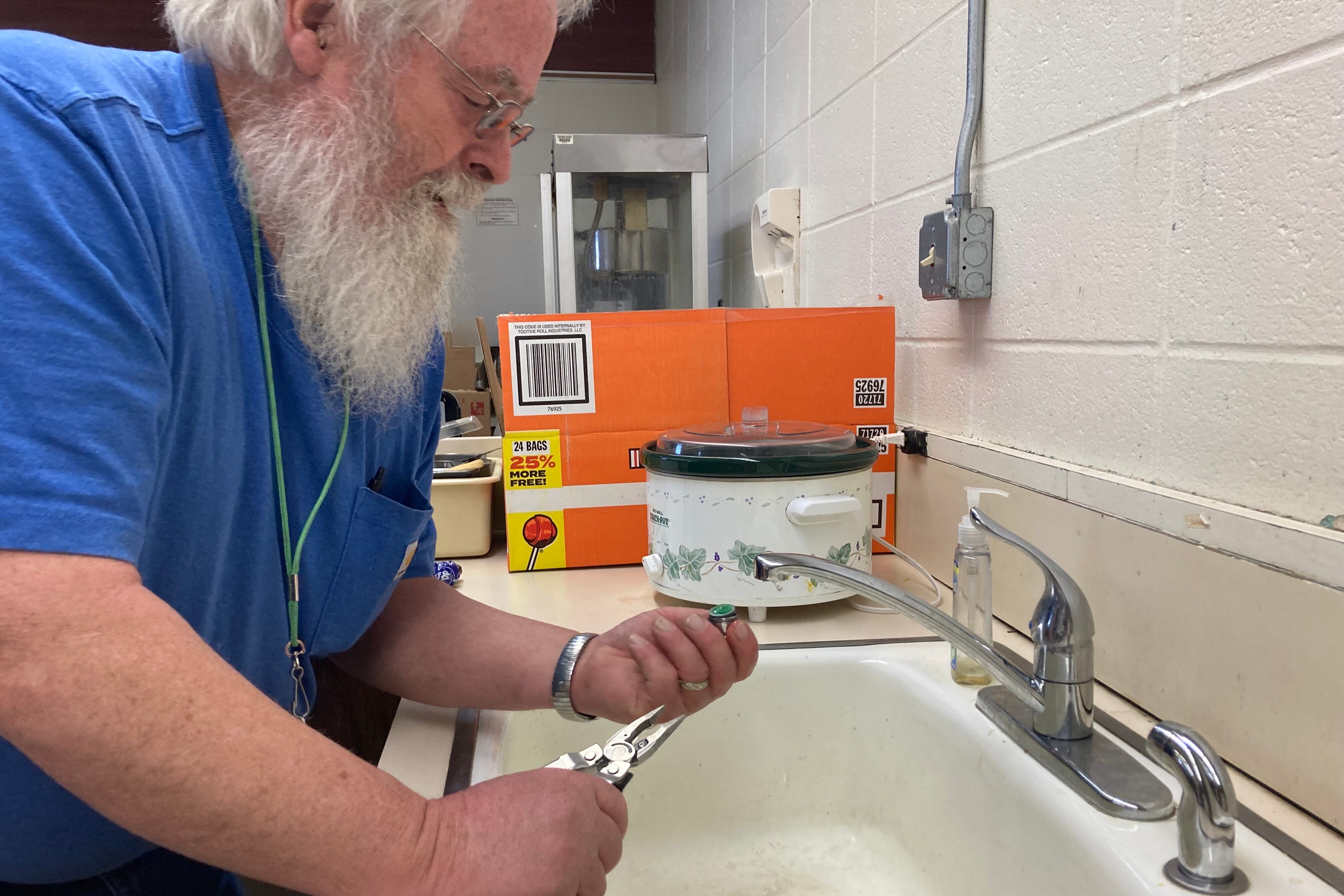
Cornelius worked to fix problem spots: new sinks in the gym locker rooms, new faucets and inlet pipes on every fixture that tested high, water bottle fill stations with built-in filtration systems like the one in the school’s lobby.
Samples from many fixtures tested safe. But some got worse, meaning in parts of the building, the source of the problem goes deeper.
Cornelius was preparing to test a third time. He plans to run the water 12 to 14 hours before the test and remove faucet filters that seem to catch grime coming from below. He hopes that will lessen the concentration enough to pass the state’s thresholds.
The EPA recommends collecting water samples for testing at least eight hours after the fixtures were last used, which “maximizes the likelihood that the highest concentrations of lead will be found.”
If the water sources’ lead concentrations come back high again, Cornelius doesn’t know what else to do.
“I have exhausted possibilities at this point,” Cornelius said. “My last step is to put up more signs or shut it off.”
KHN correspondent Rachana Pradhan contributed to this report.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.