This is a guest essay for Healthbeat. Public health, explained: Sign up to receive Healthbeat’s free national newsletter here.
Experts are growing increasingly worried that bird flu — avian influenza H5N1 — will evolve into a strain that causes widespread illness and death in humans and that the federal government is neither sufficiently containing the epidemic in animals, nor preparing sufficiently for widespread human illness.
While containment, preparedness, and overall response for national epidemics are inherently federal government responsibilities in the United States, there is one critical intervention that states and large cities should take now: Improve indoor air quality in schools and congregate settings.
State of bird flu epidemic: Threat is growing
The number of mammal species that can be infected is growing. While animal illness and deaths have been primarily in those in the wild or raised for food, infections are now spreading to household companions, such as cats, including two recent cases in New York City, and there is concern of infection spreading both human-to-pet and from pet-to-human.
Until now, most humans in the United States have been infected through close contact with an infected animal with only 70 cases (as of Tuesday). It is likely that many more infections have occurred but not been diagnosed and counted. Evolutionary changes in the virus suggest that it has a high likelihood of evolving into a strain that humans can spread to each other through the air.
To date, public concern has largely focused on food prices, food safety, and the health of pets. Experts have been focused on improving biosecurity on farms; improving surveillance in animals, humans, the environment, and food; and development of vaccines for chickens, cows, and humans. Across these discussions, the extreme impact that the Covid-19 pandemic had on all aspects of the country remains front and center.
Harms of virus vs. harms of virus-control measures
Central to the ongoing, intense debate about whether the U.S. Covid-19 response was too aggressive or not aggressive enough is the question: How does government balance the harms of the virus against the harms of virus-control measures? Between those that believe government did too much and those that believe government did too little, there are two areas of broad consensus:
- Government should have done more to protect people living in nursing homes and assisted-living facilities from the harms of the virus.
- Government should have done more to continue in-person schooling and protect children from the harms of the virus-control measures.
If H5N1 leads to a pandemic, governments will face an extreme challenge again protecting those most vulnerable to severe illness and death and ensuring that in-person schooling continues. Notably, there is one intervention that can substantially help with both: improving indoor air quality.
Why does indoor air quality matter for infectious diseases?
Infectious diseases that transmit through the air have the greatest potential to cause pandemics and impair health and wealth, because one human can readily infect multiple susceptible humans during a single interaction.
Infectious disease control over the past 100 years has focused primarily on developing medical interventions (e.g., vaccines, antimicrobials), or stopping transmission through direct physical contact (e.g., handwashing, gloves, condoms), surfaces and materials (e.g., sterilizing equipment, cleaning surfaces), and consumables (e.g., water, food). Far less has been invested in ensuring that air — particularly indoor air — is made as safe and clean as surfaces, hands, water, and food.
How do we clean indoor air?
There are three general approaches to cleaning air. The first is ventilation: ensuring that new air replaces old air. One reason infectious diseases do not transmit efficiently outdoors compared to indoors is that there is a constant supply of new air (i.e., air free from infectious disease particles) to blow away old air (i.e., air that may contain infectious disease particles). In indoor settings, ventilation can be improved by opening windows and ensuring that central air systems pull old air out and push new air in frequently.
The second approach is through filtering air. Air can be blown by a fan through a filter that traps infectious disease particles, and the air that leaves the filter is considered fresh. These filters can either be installed in centralized air systems or in portable air purification devices.
The third approach is to disinfect the air by using ultraviolet energy (known as “germicidal UV”) to inactivate or kill infectious organisms in the air.
Studies performed in laboratories and real-world settings have conclusively demonstrated that all three of these approaches work on their own and synergistically to disinfect air and reduce human infections from airborne viruses (measles, influenza, Covid-19), bacteria (tuberculosis), and fungi.
The most recent comprehensive high-quality review of indoor air quality was conducted as part of The Lancet Commission on Covid-19, which concluded that indoor air-quality improvements can reduce transmission of Covid-19 and other respiratory infectious diseases in schools and congregate settings. In this review, they also highlighted additional benefits to overall health and cognition, beyond preventing respiratory infections, from these interventions.
Invest in indoor air in congregate settings and in schools
Covid-19 demonstrated the critical importance of improving indoor air in congregate settings and in schools. Covid-19 spread wildly through assisted-living facilities and skilled nursing homes and caused over 200,000 deaths. Many infections and deaths in these facilities could have been greatly reduced by improving indoor air-quality measures.
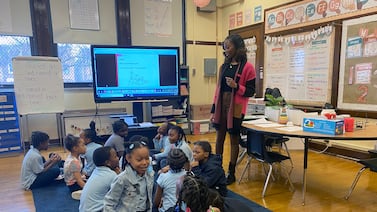
Much of the backlash against Covid-19 control measures focused on the closure of in-person schooling. Without in-person learning, children have impaired social, emotional, cognitive, and physical development, and many lose access to food and nutrition. Parents face difficulty working (either in-person or remotely), which directly impairs the economy.
The backlash against virus control measures in schools crossed the political spectrum and greatly eroded trust in government policies and institutions. Parents were angry at health and school officials; teachers were angry at parents and school officials; students became depressed; and elected officials fomented this anger to advance their political agendas.
Without question, the United States will struggle to implement and maintain an effective all-of-society response against a future H5N1 influenza epidemic unless schools are made as “pandemic proof” as possible. Keeping schools open and safe during a future emergency would greatly improve public trust in health experts and government.
What should states do now?
One of the most important pandemic preparedness initiatives after Covid-19 emerged was the White House Summit on Indoor Air Quality, which led to detailed guidance from the Centers for Disease Control and Prevention and the Environmental Protection Agency that never existed before. Industry, expert groups, and academic centers have also published detailed guidance on what governments and building operators can do. In most situations, states and cities will need to enact laws and regulations, and allocate funding for upgrading facilities and monitoring compliance.
The question most people ask is: Why make the investment in new regulations and building upgrades if we are not certain there will be a bird flu epidemic, particularly when there is a movement to shrink the size and budget of government?
The answer is that we know these investments will benefit health and productivity even if there is never a bird flu epidemic. They can help us reduce the spread of routine seasonal airborne flu and Covid-19, as well as outbreaks of measles. They will reduce the impact of allergies and pollution. They will protect people when there are wildfires.
The time to prepare our defenses is now.
Dr. Jay K. Varma is a physician and epidemiologist. An expert in the prevention and control of infectious diseases, he has led epidemic responses, developed global and national policies, and implemented large-scale programs that saved hundreds of thousands of lives in Asia, Africa, and the United States.
Healthbeat is a nonprofit newsroom covering public health published by Civic News Company, which also publishes Chalkbeat. Sign up for Healthbeat’s newsletters here.